Is Minimally Invasive Dentistry Right For You?
Minimally Invasive Dentistry has become quite popular recently. Dentists around the world have encouraged their patients and shared their positive opinions about this interesting technique. Minimally Invasive Dentistry is recommended for everyone, but especially for those of you who believe it is better to prevent than to treat illnesses and diseases. For today’s blog, we have chosen to talk about the importance of Minimally Invasive Dentistry and what it means for our patients. Hopefully, Dr. Galaif’s blog will encourage you to take steps toward this amazing dental procedure in the future.
Minimally Invasive Dentistry, or Microdentistry, is the application of “a systematic respect for the original tissue.” The goal is to conserve healthy tooth structure. It focuses on prevention, remineralization, and minimal dentist intervention. Using scientific advances, Minimally Invasive Dentistry allows Dr. Galaif to perform the least amount of dentistry needed, while never removing more of the tooth structure than is required to restore your teeth to their normal condition. In addition, in Minimally Invasive Dentistry, dentists use long-lasting dental materials that conserve the maximum tooth structure, so the need for future repairs is reduced.
What is Minimally Invasive Dentistry?
It is a term that includes numerous procedures, all of which are performed with the single aim to conserve and improve the patient’s oral health, providing healthy tooth structure. The term itself – Minimally Invasive Dentistry explains how dentists who use this approach focus on removing as little as possible when it comes to the tooth structure, while at the same time getting rid of the problem and improving your oral health in general.
How does it work?
Minimally Invasive Dentistry not only prevents common dental issues, it also analyzes and evaluates any possible risks and identifies problems in early stages. Dr. Galaif will first evaluate your risk for tooth decay. The presence of bacteria, quality and quantity of saliva, and your diet all contribute to potential tooth decay. Dr. Galaif and his team will then use strategies to prevent or reduce your risk for tooth decay. For instance, if you have a high level of oral bacteria, you might be advised to use mouthwash daily, limit the intake of certain carbohydrates, and practice good oral hygi ene. With Minimally Invasive Dentistry, Dr. Galaif and his staff provide a chance to reduce the need for future dental repairs, achieved by using long-lasting materials and the least amount of dentistry which is also highly efficient at the same time. In order to do so, Dr. Galaif will perform series of tests in order to determine important highlights, such as the number of healthy bacteria in your saliva and the presence or absence of tooth decay and caries.
ene. With Minimally Invasive Dentistry, Dr. Galaif and his staff provide a chance to reduce the need for future dental repairs, achieved by using long-lasting materials and the least amount of dentistry which is also highly efficient at the same time. In order to do so, Dr. Galaif will perform series of tests in order to determine important highlights, such as the number of healthy bacteria in your saliva and the presence or absence of tooth decay and caries.
Here are some of the Minimally Invasive Dentistry options:
Air abrasion
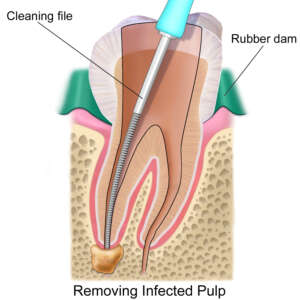
Air abrasion is a drill-less technique used to remove tooth decay, and it can perform other procedures too. The technique uses a stream of aluminum oxide particles generated from compressed air, or helium. These abrasive particles use a high velocity to act on a tooth and remove a small concentration of its structure. Hardness of the material or tissue being removed influences efficacy of air abrasion. Parameters of the device used to perform air abrasion also contribute to effectiveness of the procedure. This Minimally Invasive technique can be used for the removal of pit and fissure surface stain on enamel before placing veneers, and can also detect caries, and remove other defects.
Remineralization
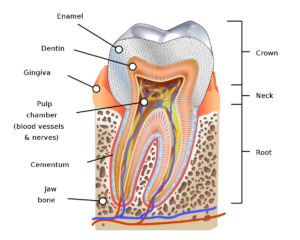
Remineralization is a process of restoring minerals, the damage that has been done due to demineralization. Demineralization is a chemical process wherein minerals, mainly calcium and phosphate, are removed from enamel, dentine, and other tissues in your mouth. Studies show that demineralization of teeth is caused by acidic attack through dietary acids consumed through food and beverages and microbial attack from bacteria present in the mouth.
When not addressed properly, demineralization can lead to caries and other problems. The gold standard in a process of remineralization is fluoride, which is why dentists recommend it to their patients, but other methods are also useful such as the use of toothpaste containing casein phosphopeptide-amorphous calcium phosphate (CPP-ACP), gums, mouthwash and other products containing xylitol.
Sealants
Dental sealants are plastic coatings used to protect the teeth from the harmful bacteria that lead to the process of tooth decay. Sealants are a safe, effective, and fast way to protect your teeth from damage, caries, and other problems. The plastic coating is applied onto the biting surfaces of the back teeth (molars and premorals). Once applied, the sealant forms a hard shield that prevents bacteria and food in small grooves in your teeth. The reason why sealants are put on molars and premolars specifically is because these teeth have small pits where food can get stuck. The process is fast, it takes only a few minutes to position a sealant on each tooth. And the entire procedure is typically pain-free. Dentists have been using sealants to cover the grooves on chewing surfaces, and now they are using them to close up lesions developing between teeth. They apply the resin onto the tooth’s surface, and a network of pores within the enamel force the resin deep into the tooth.
Bite Splints
Bite splints are created to prevent damage from teeth grinding, especially at night. Bite splints are hard plastic wafers specifically designed to fit over upper teeth. The primary purpose of bite splints are to stop you from grinding the teeth or bruxism, which is something that most people do while they sleep. This habit wears down tooth enamel and makes it prone to damage. At first, wearing a bite splint may be unusual or awkward, but you’ll get used to it. Proper care is mandatory so always make sure you keep the bite splint in a container with a little cold water to prevent it from drying out.
Inlays and Onlays
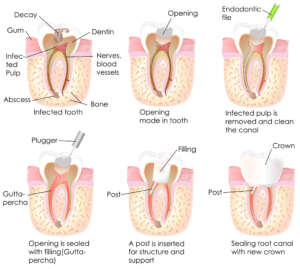
Inlays and Onlays are used to restore the form of the teeth after a certain procedure has been performed, such as removal of caries. These restorations are generally used to repair back teeth with mild to moderate decay. They also prove to be useful when addressing cracked or fractured teeth that aren’t damaged to a degree that requires a crown. Patients with too much tooth damage and decay that can’t be fixed with a filling are ideal candidates for Inlays and Onlays. A major benefit of these restorations is their durability as well as the ability to strengthen teeth.
What are the advantages of Minimally Invasive Care?
Minimally Invasive Care has many benefits, especially for patients, as it includes simple treatment options that can reduce anxiety and result in better long-term outcomes. Minimally Invasive Care treatments, which are often less expensive, include diagnostic solutions, fluorides, antimicrobials, regeneratives, and therapeutic fillings and sealants. For patients, these options are far more desirable and accessible than expensive and painful needles, drills, and extractions. Minimally Invasive options can also help patients (and providers) avoid the cycle of repairs and procedures that are often needed with other restorative work.
Minimally Invasive Dentistry focuses on not only treating common dental issues, but also on preventing and reducing the risks of these issues. By using high quality, long lasting materials, sharing basic tips on how to take care of your oral health, reminding you to check in with Dr. Galaif regularly and discover any problems while it still in their early stages, Minimally Invasive Dentistry is a very positive option and approach which is valued by dentists and accepted by patients who have enjoyed successful results.
Give Dr. Galaif a call at (818) 789-6789 to learn more about Minimally Invasive Care options that we offer.
You can also visit the appointment page on our Web site: