Do You Or Someone You Know Suffer From TMJ Pain?
The temporomandibular joints (TMJ) are the 2 joints that connect your lower jaw to your skull, one on each side. They are the joints that slide and rotate in front of each ear, and consist of the mandible (the lower jaw) and the temporal bone (the side and base of the skull). You can feel them by placing your fingers in front of your ears and opening your mouth.
The TMJ’s are among the most complex joints in the body, which along with several muscles allow the mandible to move up and down, side to side, and forward and back. When the mandible and the joints are properly aligned smooth muscle actions, such as chewing, talking, yawning, and swallowing are able to take place. When these structures (muscles, ligaments, disk, jaw bone, temporal bone) are not aligned, or synchronized in movement, problems may occur.
Temporomandibular disorders (TMD) are disorders of the jaw muscles, temporomandibular joints (TMJ), and the nerves associated with chronic facial pain. Any problem that prevents the complex system of muscles, bones, and joints from working together in harmony may result in temporomandibular disorder (TMD).
There are three main classes of TMDs:
- Disorders of the joints, including disc disorders
- Disorders of the muscles used for chewing (masticatory muscles)
- Headaches associated with a TMD
The National Institute of Dental and Craniofacial Research classifies TMD by the following:
- Myofascial Pain (the most common form of TMD), resulting in discomfort or pain in the fascia (connective tissue covering the muscles), and muscles that control jaw, neck and shoulder function.
- Internal Derangement of the Joint – which means a dislocated jaw or displaced disk (cushion of cartilage between the head of the jaw bone and the skull), or injury to the condyle (the rounded end of the jaw bone that articulates with the temporal skull bone).
- Degenerative Joint Disease, which includes osteoarthritis or rheumatoid arthritis in the jaw joint.
It is possible to have one or more of these conditions at the same time. The exact cause of a person’s TMJ disorder may be difficult to determine. Your pain may be due to a combination of factors such as genetics, arthritis or jaw injury. Sometimes the main cause is excessive strain on the jaw joints and the muscle group that controls chewing, swallowing, and speech. This strain may be a result of habitual, involuntary clenching or grinding of your teeth (bruxism), although some people who clench or grind their teeth never develop TMJ disorders. Trauma to the jaw, the head, or the neck may also cause TMD. Arthritis and displacement of the jaw joint disks can cause TMJ pain. In other cases, another painful medical condition such as fibromyalgia or irritable bowel syndrome may overlap with or worsen the pain of TMD. The National Institute of Dental and Craniofacial Research has identified clinical, psychological, sensory, genetic, and nervous system factors that may put a person at higher risk of developing chronic TMD.
A recent study found that about 11 to 12 million adults in the United States have had pain in the region of the temporomandibular joint (TMJ). Temporomandibular disorders (TMD) are twice as common in women than in men, especially in women between the ages of 35 and 44 years old. In most cases, the pain and discomfort associated with TMJ disorders is temporary and can be relieved with self-managed care or nonsurgical treatments. Surgery is typically a last resort after conservative measures have failed, but some people with TMJ disorders may benefit from surgical treatments.
The following are the most common signs and symptoms of TMD:
- Jaw discomfort or soreness
- Headaches or migraines
- Pain spreading behind the eyes, in the face, shoulder, neck, and/or back
- Pain in and around your ear, earaches or ringing in the ears (not caused by an infection of the inner ear canal)
- Aching facial pain or swelling on the side of your face
- Toothache
- Pain or tenderness of your jaw
- Painful clicking, popping, or grating in the jaw joint when opening or closing your mouth
- Locking of the joint, making it difficult to open or close your mouth
- Limited mouth motions
- Difficulty chewing or pain while chewing
- Clenching or grinding of the teeth
- Dizziness
- Sensitivity of the teeth, without the presence of an oral health disease
- Numbness or tingling sensation in the fingers
- A change in the way the upper and lower teeth fit together
TMJ disorders can cause a clicking sound or grating sensation when you open your mouth or chew. But if there’s no pain or limitation of movement associated with your jaw clicking, you may not need treatment for a TMJ disorder. The symptoms of TMD may look like other conditions or medical problems. Make an appointment with Dr. Galaif for an accurate diagnosis.
The best treatment will based on how old you are; your overall health and medical history; how well you can handle specific medicines, procedures, or therapies; how long the condition is expected to last; and your opinion or preference. Dr. Galaif will note your symptoms, and take a detailed medical history. He will ask questions about your pain, including its location, when it occurs, what makes it better or worse, and if it stays in one area or spreads to other parts of your body. Dr. Galaif will also ask if you have other pain conditions such as headache or back pain, and examine your head, neck, face, and jaw for tenderness; jaw clicking or popping; or difficulty with movement. He may also suggest imaging studies such as an X-ray, Magnetic Resonance Imaging (MRI), or Computed Tomography (CT).
Treatment(s) may include:
* Resting the Temporomandibular Joint (TMJ)
* Medicine or pain relievers
* Moist heat or cold packs
* Relaxation techniques and/or stress management
* Physical therapy, ultrasound or biofeedback
* Acupuncture
* Diet changes (soft foods to rest the jaw muscles, avoiding hard and crunchy, or chewy foods)
* Behavioral changes (including things like improving posture, not holding a phone between your shoulder and ear)
* Limit extreme jaw movements (keeping yawning and chewing, especially gum or ice to a minimum, don’t yell, sing, or do anything that forces you to open wide)
* Trigger point injections
* Transcutaneous Electrical Nerve Stimulation (TENS, using low-level electrical currents to relax your jaw muscles)
* Surgery
Dr. Galaif may also recommend an intraoral appliance to reduce teeth grinding (a device that fits over your teeth, but does not change the teeth or your bite). These appliances are also known as nightguards, splints, occlusal splints, interocclusal splints, or bruxism splints.
TMJ Implants are artificial devices that are used to replace part of the jaw joint or the entire joint. Implants might be considered when:
- There is an injury to the joint
- There is a condition you’re born with (congenital condition) that needs to be repaired
- The joint is frozen (ankylosis), commonly caused by injury or infection
- There’s severe damage to the joint
- There’s ongoing pain
- All simpler treatments have been tried, and have failed
In certain cases, TMJ implants can improve function and quality of life.
There are several types of over-the-counter (OTC) and prescription medications that can ease TMJ symptoms, including:
* Pain relievers like acetaminophen
* Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen
* Muscle relaxers (particularly helpful for people who clench or grind their teeth)
* Antidepressants (which can change how your body interprets pain)
If you are concerned about TMJ or TMD issues, or if you have other oral health concerns,
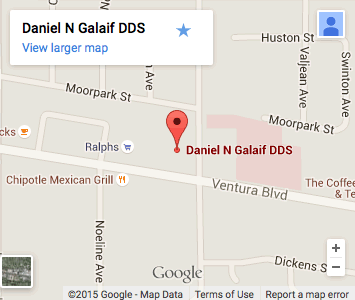
give us a call at (818) 789-6789 to make an appointment for the highest quality dental care.
You can also visit the appointment page on our Web site: